Single
Ventricle
Palliation
-
![]()
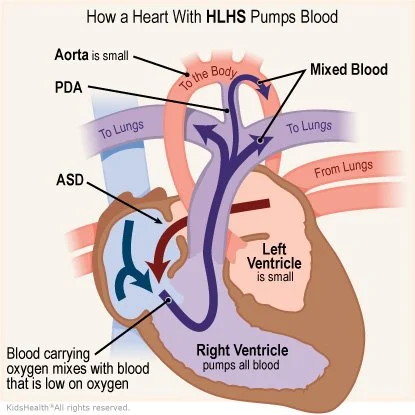
What is "Hypoplastic Left Heart"?
Expected O2 sat: 70-80%
Hypoplastic left heart syndrome (HLHS) is a congenital heart defect in which the left side of the heart and unable to function properly. This results in inadequate oxygenation and circulation of blood to the body.
Without treatment, HLHS is usually fatal within the first few weeks of life. The treatment of HLHS typically involves a series of surgeries that aim to reroute blood flow to the body through the right ventricle, which is larger and able to handle the workload of the entire circulatory system. This is known as "single ventricle palliation,” which involves multiple stages over the course of several years.
In the first hours of life, it is crucial to have left to right atrial shunting (usually ASD, or sometimes a decompressing vein) and PDA. Lack of ASD or PDA is incompatible with life as there is no other way to get oxygenated blood to the systemic circulation. Early administration of prostaglandin and atrial septectomy are essential.
You should expect LOW sats (70-80%) due to mixing. If you are getting >95%, then you have too much blood going to the lungs (high Qp/Qs ratio) and essentially stealing from the systemic circulation. This can lead to NEC, decreased brain development, and shock.
-
![]()
Stage 1: Norwood
Expected O2 sat: 75-85%
During the first stage of the procedure, typically done within the first few weeks of life, a shunt is placed between the pulmonary artery and the aorta to improve blood flow to the lungs. This is called a "Blalock-Thomas-Taussig (BTT) shunt. Then the surgeon creates a new aorta by reconstructing the pulmonary artery and connecting it to the systemic circulation. This allows the right ventricle of the heart to take over the function of the left ventricle. All together this procedure is called the “Norwood” procedure:
1. DKS Anastamosis combines aorta and PA to make neoaorta to create a systemic outflow tract
2. BTT Shunt (innominate artery to PA) or Sano shunt (RV to PA)
3. PDA ligation
Complications:
BTT shunts are continuous flow in systole/diastole so you can get low diastolic BP and coronary steal. Sano shunts pump with systole so there is no risk of coronary steal.
BT shunts can also clot. If the patient is desatting, listen for shunt murmur and notify cardiology ASAP (may need transfer to CICU for heparin bolus to dislodge clot).
As the baby grows, pulmonary vascular resistance (PVR) drops and your pulmonary circulation (Qp) increases through the shunt leading to pulmonary over-circulation requiring advancement to the next stage of palliation.
-
![]()
Stage 2: Glenn
Expected O2 Sat: 80-85%
In the second stage, which is usually performed between four and six months of age, the shunt is replaced with a more permanent connection between the pulmonary artery and the superior vena cava. This procedure is called the "Glenn" procedure:
Connect SVC to PA
Complications:
If there are problems with the Glenn circuit, you can see increased head circumference and findings similar to SVC syndrome due to the passive flow leading to backup. May presents as a headache with enlarged head circumference.
Hepatic factor needs to get to the lungs to promote lung function. The Glenn circuit prevents hepatic factor from getting to the lungs resulting in pulmonary arteriovenous malformations which leads to V/Q mismatch and hypoxia. This continues to be a risk in the long term (not just 4-6 months out)
If there is not enough pulmonary blood flow, aortopulmonary collaterals may form. Can also see venous-venous collaterals if pulmonary pressures rise
-
![]()
Stage 3: Fontan
Expected O2 Sat: >85%
The third and final stage, typically performed between 18 months and three years of age, involves the connection of the inferior vena cava to the pulmonary artery, bypassing the heart entirely. This is called the "Fontan" procedure:
1. Connect IVC to PA (can be intra/extracardiac or extracardiac)
2. Fenestration from IVC to RA : Acts as a pop-off valve to allow offloading of increased pressures
Complications: With Fontans, the CVP is always equal to the mean PA pressure (which is higher than a normal CVP) and can lead to:
Protein-losing enteropathy (diarrhea, low albumin)
Chylous effusions/Plastic bronchitis (pleural effusions)
Sinus node dysfunction leading to atrial arrhythmias and junctional rhythms
Liver dysfunction/cirrhosis
Coagulopathy, ascites, effusions, edema and many other complications like ADHD, clotting, and exercise intolerance.